Supercharge every phase of micromedical device product development with these questions.
First, some of the biggest considerations for designing, manufacturing and scaling today’s smaller, smarter medical innovations center on providing power to microelectronic systems.
From mechanical functionality to data operations and wireless communications, effective power management drives continued device innovation. Addressing five fundamental issues can help multidisciplinary teams bring new and next-generation medical devices to market on-time and on-budget.
1: Why: The use case
The obvious starting point is documenting the intended use. Why is a product being built and how will it be used? A single-use device for specialized clinical procedures will have different power requirements than reusable biosensors in consumer settings.
Additionally, how long will a device be used — from minutes to years — and is it part of a focused diagnostic protocol or ongoing treatment regimen? All of these factors matter for effective power management.
With market demand accelerating for smaller, smarter devices functioning in networked environments, an engineering mandate now is a growing need for always- on, no-fail wireless communications for supporting secure access to accurate, timely data. Clearly defining the use case for data operations in the earliest stages of R&D is of critical importance. to market on-time and on-budget.
2: How: Power supply and power budget
As key use case requirements come into focus, the next step is how the device will be powered. Will it be a single-use device or multi-use with replaceable batteries? Or perhaps the device itself is rechargeable, which is becoming more and more common.
There are almost always trade-offs. If a device is disposable, it will most likely need to ship fully charged. But if it’s rechargeable, it will either need electromechanical functionality (e.g., pins) or wireless (e.g., inductive, RF, etc.). Replaceable batteries call for battery contacts, access doors and other parts. Battery chemistry and the environmental costs of disposal are topics of increasing importance.
Functionally, a critical consideration is understanding peak current requirements and the expected duration between recharge or replacement and then matching it to supply capability. This is the power budget, normally specified in watts (W). Calculations are in the format of a spreadsheet where input voltage, input current, output voltage, output current, power in and power out are documented for each power stage and electronics load. Typical electronics load components can include power conversion/conditioning, A to D and D to A conversion, digital signal processing, memory, wireless radios, sensors and perhaps output transducers or displays.
Think of a power budget as a swimming pool with a leaking drain and a resupply hose. The pool represents the battery, the resupply hose represents recharging or replacing the battery and the leaky drain represents all the electronic loads. The trick is designing the pool so it’s large enough that the drains last long enough for the intended use, and so the resupply hose is big enough that the pool never empties. Think “balance“.
3: What: Components and board design The main focus at this stage is control. Do users manually put the device into sleep mode for power conservation, or is there a timer? How do users monitor the battery life, or is that controlled by software?
Onboard wireless technology influences component selection and board design because it’s often one of the biggest parts of the power budget, from start-up to steady state conditions. The power source and power conditioning must be able to supply enough current to fulfill the inrush of current when the circuit starts up, but also handle transient demands in use.
Over the long haul, the power supply must be large enough to last through the entire intended use scenario, but not so large as to result in physical space constraints or excess costs (upfront materials costs as well as end-of-life environmental costs and all the maintenance costs in- between). This mandate could range from minutes or hours to months or even years.
4: When: Now! More data, more ways
Data is the driver. As the medical device market continues to advance, software and firmware are foundational for building stable, secure platforms. Effective power management is the behind-the-scenes safeguard that secures new product acceptance and long-term success.
Consider electrocardiogram (ECG) monitors. Historically they were offline devices that collected and stored data that often took days to review. Even then, it wasn’t uncommon for a lab to receive limited data due to lead connection problems. Today, data analysis occurs in real time through wireless communications. This accelerated timeframe places new demands on power management to accommodate data processing, the displays and cloud connectivity.

5: Where: Materials supply and disposal
There’s no margin for error with a medical device in terms of dependability. It simply has to work — and that goes for supply chains to support high-volume manufacturing.
The effects of COVID on supply chains for medical electronics are still being felt. Everything from components (such as resistors and inductors) to complicated
ICs have been in short supply with prices and lead times skyrocketing. Many manufacturers have resorted to stockpiling excess inventory. Product redesign initiatives have necessitated revalidating processes and submitting market clearance documentation to regulatory bodies.
On the downstream end, safe disposal is critical because batteries may contain toxic heavy metals. Recycling is ideal, but uptake is inconsistent and proper handling is difficult to enforce. As a result, it’s important that medical devices are designed with the smallest batteries available that meet the demands of the use case.
6: Who: The partnership accelerant
When power management is at its most efficient it is as invisible as electricity itself. High-performance R&D teams function much the same way, directing the flow of energy capably and smoothly for maximum effect.
Close collaboration with internal colleagues as well as external partners supercharges every phase of development, empowering new breakthroughs in performance as medical devices keep getting even smaller and smarter.
About Intricon
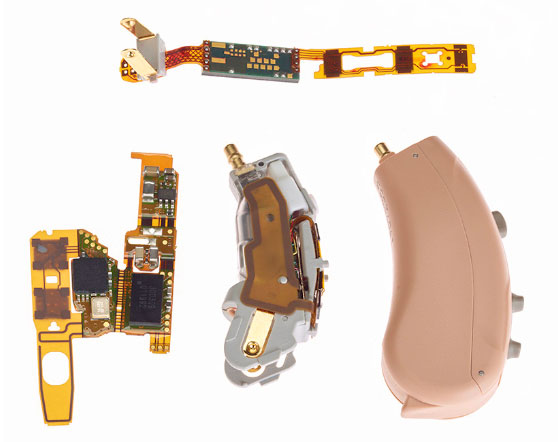
For four decades, Intricon has improved and extended people’s lives by developing and manufacturing sensor- driven micromedical devices. Intricon partners with medical device companies, providing unique microelectronic expertise—including miniature molding through final assembly – and regulatory guidance, supply chain optimization, and scalable production, exclusively for the medical market. Intricon brings the world’s smallest, smartest new and next generation devices to life.